The realm of bacterial infections has been an area of interest for researchers for years, with meningitis being one of the deadliest diseases that arise due to the infection of the meninges. The latest research published in the journal Nature has shed new light on how bacteria exploit pain-sensing nerve cells to invade the brain and cause meningitis.
Meningitis: A Life-Threatening Condition
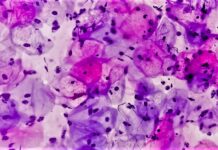
Meningitis is a severe disease that is characterized by inflammation or stroke, which can be life-threatening. It is a rare condition, but it has a high mortality rate of up to 30% of patients. Thus, the development of therapies to combat meningitis has been a critical area of focus for researchers.
The Pain Pathway Exploited by Meningitis Bacteria
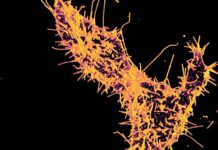
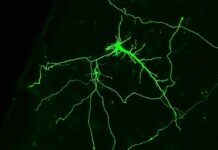
The researchers in the latest study used genetic engineering techniques to create mice without pain neurons, which showed more effective results in fighting bacterial infections than normal mice. However, during the infection, they found that pain fibers suppress immune cells in the dura, which is a key barrier site. Further research uncovered that a molecule called CGRP, released by pain-sensing neurons, plays a crucial role in suppressing immune cells during bacterial meningitis.
Implications of the Research Findings
The findings of this research have significant clinical implications, as CGRP blockers are already clinically available and safe to use in humans. CGRP blockers can modulate immunity before the onset of the disease, which makes it a potential treatment for meningitis. However, the researchers note that CGRP antagonists alone might not be enough to treat meningitis, as the mice eventually died from the infection.
Unraveling the Mystery of Meningitis Infection
Despite the promising findings, there are still several unanswered questions about why CGRP suppresses immune cells in the dura, and how bacteria exploit this mechanism to infiltrate the brain better. The researchers believe that there may be a protective mechanism in place to prevent inflammation from getting out of control near the brain and causing damage. However, bacteria have evolved to take advantage of this mechanism, allowing them to cause meningitis.
The Future of Meningitis Treatment
While the study’s findings offer new insights into how bacteria infiltrate the brain and cause meningitis, applying these findings directly to treatment may be challenging. Nevertheless, the discovery of CGRP blockers as a potential modulator of immunity is an exciting development. More research is needed to fully understand the mechanisms behind bacterial meningitis and develop more effective treatments.
Conclusion
In conclusion, this study provides a deeper understanding of how bacteria can infiltrate the brain and cause meningitis by exploiting the pain-sensing nerve cells. The study’s findings have important clinical implications, and with further research, we may be able to develop more effective strategies for combating meningitis and other bacterial infections in the future. The complex and intricate nature of meningitis infection and its treatment continue to be an area of interest and critical research.
Google News | Telegram