An Unveiling of a Groundbreaking Discovery
Embarking on a groundbreaking journey, recent research has shed light on an enigmatic pathway within the immune system that orchestrates the emergence of withdrawal symptoms in individuals grappling with opioid addiction. Delving deep into the intricate tapestry of the human body, scientists have unearthed a remarkable interplay between the immune system, the central nervous system, and the elusive blood-brain barrier. This revelation not only expands our understanding of withdrawal but also paves the way for novel interventions that hold the potential to prevent withdrawal and facilitate the recovery process for those ensnared by the clutches of opioid dependency.
The Untold Connection: Immune System’s Enigmatic Bond with Withdrawal
While previous studies have hinted at the involvement of the immune system in the intricate realm of opioid withdrawal, a recently published study in the esteemed journal Cell has now forged an undeniable connection between the immune system, the formidable blood-brain barrier, and the bewildering symphony of withdrawal symptoms. This momentous study unravels a treasure trove of clinical avenues that could potentially revolutionize the landscape of addiction treatment, providing a glimmer of hope for individuals yearning to taper off opioids safely and embark on a path of lasting recovery.
Penetrating the Mechanistic Enigma
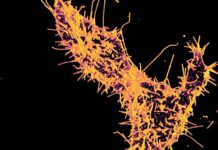
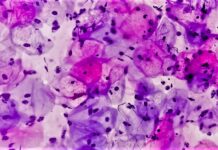
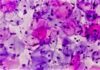
Venturing deep into uncharted territories, researchers meticulously analyzed blood samples from 21 individuals ensnared by the grasp of heroin addiction, juxtaposed against 20 control subjects untainted by opioids. The remarkable findings illuminated a stark contrast, with the immune systems of heroin users showcasing biomarkers suggestive of profound immune system dysfunction. Employing cutting-edge flow cytometry experiments, scientists made the startling discovery of elevated levels of a peculiar immune cell variant, christened as fragile-like regulatory T cells (Tregs), permeating the bloodstream of the heroin-using cohort. While Tregs typically exert immunosuppressive properties, these atypical counterparts existed in an unprecedented fragile-like state, unleashing an inflammatory cytokine called interferon-γ (IFN-γ). Intriguingly, the study postulates that the abnormal state of these Tregs could be attributed to the harrowing consequences of opioid-induced hypoxia.
Mouse Models: Breathing Life into the Findings
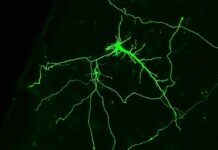
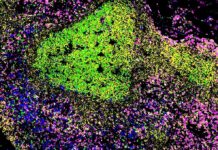
To validate and breathe life into their remarkable discoveries, scientists turned to an unconventional cohort—mice. Administering heroin to these unsuspecting creatures, researchers bore witness to a surge in fragile-like Treg cell counts and a surge in IFN-γ expression coursing through their veins. However, the true revelation lay within the inner sanctum of the brain—the nucleus accumbens—a pivotal region intricately woven into the intricate fabric of addiction. Astonishingly, samples derived from the mice unveiled the presence of IFN-γ not only within their bloodstream but also within the nucleus accumbens, fueling speculation that these delicate Treg cells have the uncanny ability to traverse the typically impervious blood-brain barrier. The study unearths a mesmerizing piece of the puzzle—the role of C-C motif chemokine ligand 2 (Ccl2) expression in neurons residing within the nucleus accumbens, orchestrating the enthralling trafficking of Tregs into the brain, further cementing the symbiotic relationship between brain cells and the immune response.
Unmasking the Impact: Unveiling the Role in Withdrawal
Intriguingly, the revelations surrounding the delicate dance between fragile-like Treg cells and the enigmatic realm of withdrawal carry profound implications. Scientists unearthed a stunning realization—the expression of IFN-γ by fragile-like Treg cells weakened the synaptic connections among neurons nestled within the nucleus accumbens, ultimately giving rise to the dreaded withdrawal symptoms in mice. Building upon this captivating insight, researchers embarked on a mission to unravel the true potential of their findings, experimenting with IFN-γ knockout mice and administering an IFN-γ-neutralizing antibody to mice before opioid administration. The results were nothing short of remarkable—preserving robust neural connections during the withdrawal phase led to a remarkable reduction in the intensity and duration of withdrawal symptoms, offering a glimmer of hope amidst the seemingly relentless storm of addiction.
Future Horizons: Paving the Path for Uncharted Explorations
As the study casts its spell on the scientific community, it becomes evident that the journey has just begun. While the findings stand as pillars of insight into the intricate mechanisms underlying withdrawal, a treasure trove of uncharted territories awaits further exploration. The next frontier beckons—a clarion call for longitudinal studies encompassing human subjects, offering a unique lens into the predictive value of fragile-like Treg cell counts in gauging the severity and duration of withdrawal. Additionally, the study humbly acknowledges the enigmatic nature of the expansion of fragile-like Tregs within the bloodstream of heroin users, urging further investigation into the role of the gut-brain axis, sepsis, and the mesmerizing neurocircuitry of addiction—paving the path for a holistic understanding of the entire captivating process.
Unlocking the Potential: Therapeutic Crossroads
Even amidst the lingering questions, this remarkable study extends an invitation to the realm of potential therapeutic targets—a realm brimming with hope and possibilities. The tantalizing potential of interventions targeting fragile-like Treg cells emerges as a promising avenue to disrupt the vicious cycle of withdrawal. Envision the uncharted—a realm where the testing of IFN-γ-blocking drugs on human opioid users, or even daringly venturing into the realm of heroin users, sheds light on the profound impact of these interventions in preventing or ameliorating withdrawal symptoms. Such bold explorations hold the key to transforming the recovery journey, casting aside the shackles of withdrawal that too often sow the seeds of relapse.
Scientist Luis Montaner, a fervent advocate of scientific exploration, proposes the dawn of longitudinal studies in humans—a groundbreaking endeavor destined to unravel the predictive prowess of fragile-like Treg cell counts in elucidating the severity of withdrawal. In this ever-evolving landscape, the exploration of archived samples from previous withdrawal studies, entangled with the presence of these elusive cells, presents an enticing path toward unlocking hidden revelations.
The Epilogue: A Journey of Boundless Potential
In the grand tapestry of scientific discovery, this study marks a momentous stride toward unraveling the enigma that shrouds the immune system’s role in opioid withdrawal. Its revelations pave the way for clinical interventions and therapeutic targets that hold the power to defy the clutches of withdrawal symptoms and forge a path toward lasting recovery. As the curtains draw close on this chapter, the echoes of promise and the fervor of exploration continue to reverberate. The path ahead teems with unexplored avenues and limitless potential, beckoning scientists to persist in their quest to address the formidable challenges posed by opioid addiction. With each stride, humanity moves closer to a brighter future—one liberated from the depths of addiction and anchored in the triumph of scientific understanding.
Google News | Telegram